Understanding Sepsis: Uncovering What Goes Wrong in the Body’s Smallest Blood Vessels
Each year, sepsis claims the lives of around 8,700 Australians, more than prostate cancer, breast cancer, or road accidents.
It can strike suddenly, turning what begins as a simple infection into a life-threatening emergency. Survivors are often left with lasting health issues and little understanding of what happened to them.
Sepsis occurs when the body’s immune response to an infection spirals out of control, triggering widespread inflammation, organ failure and, too often, death. Despite its severity, there is still limited evidence to guide the clinical management of sepsis. Current treatments focus largely on managing symptoms through antibiotics, fluids and medications to support blood pressure, rather than addressing the underlying disease processes themselves.
This is where a RPH Research Foundation-funded research project is making a critical contribution.
Led by Dr Erika Bosio, the project focuses on understanding what happens to the body’s microvasculature, the smallest blood vessels in the body, during sepsis. These tiny vessels play a vital role in maintaining circulation and delivering oxygen to organs, yet they are among the first systems to fail when sepsis takes hold.
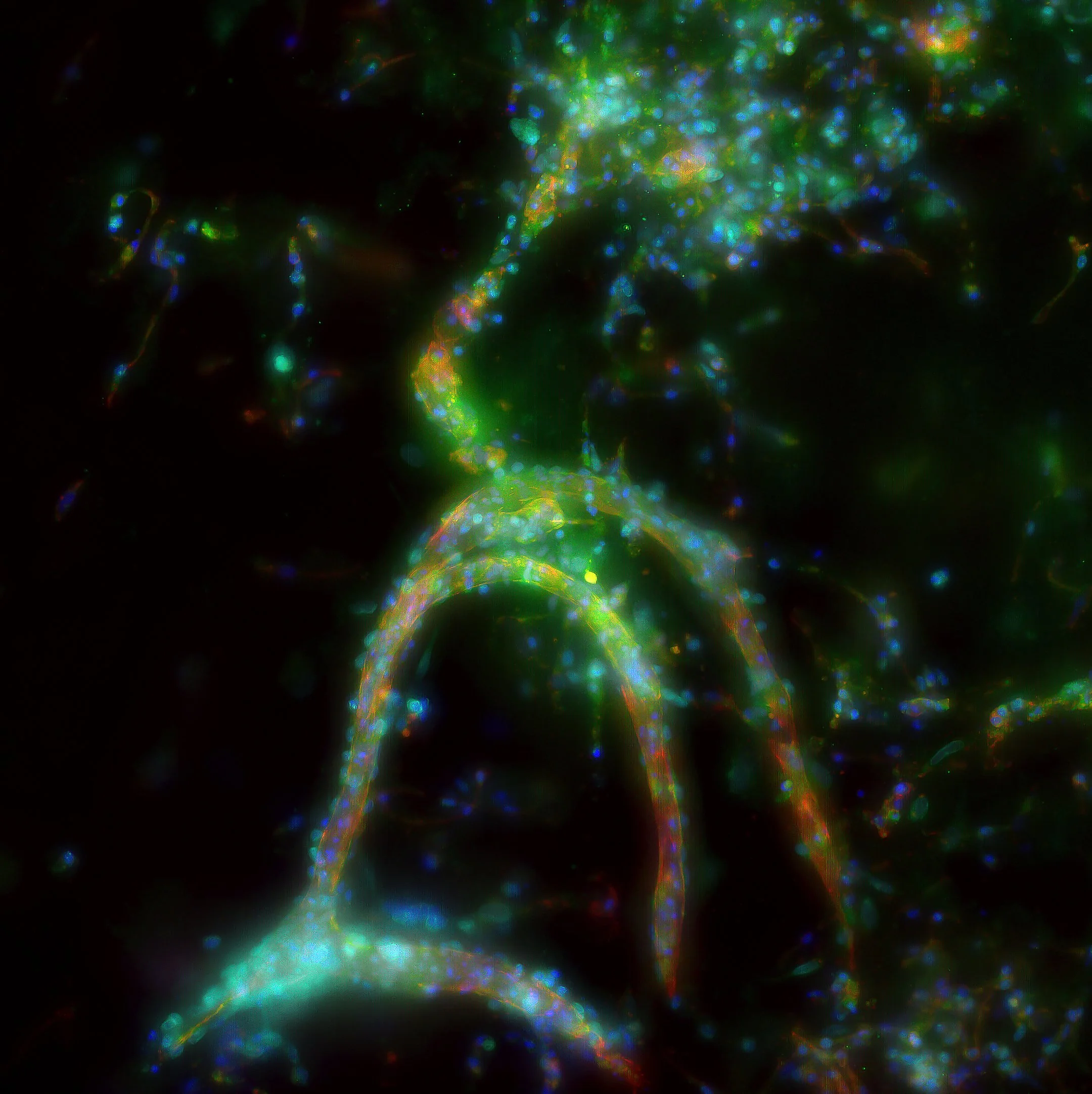
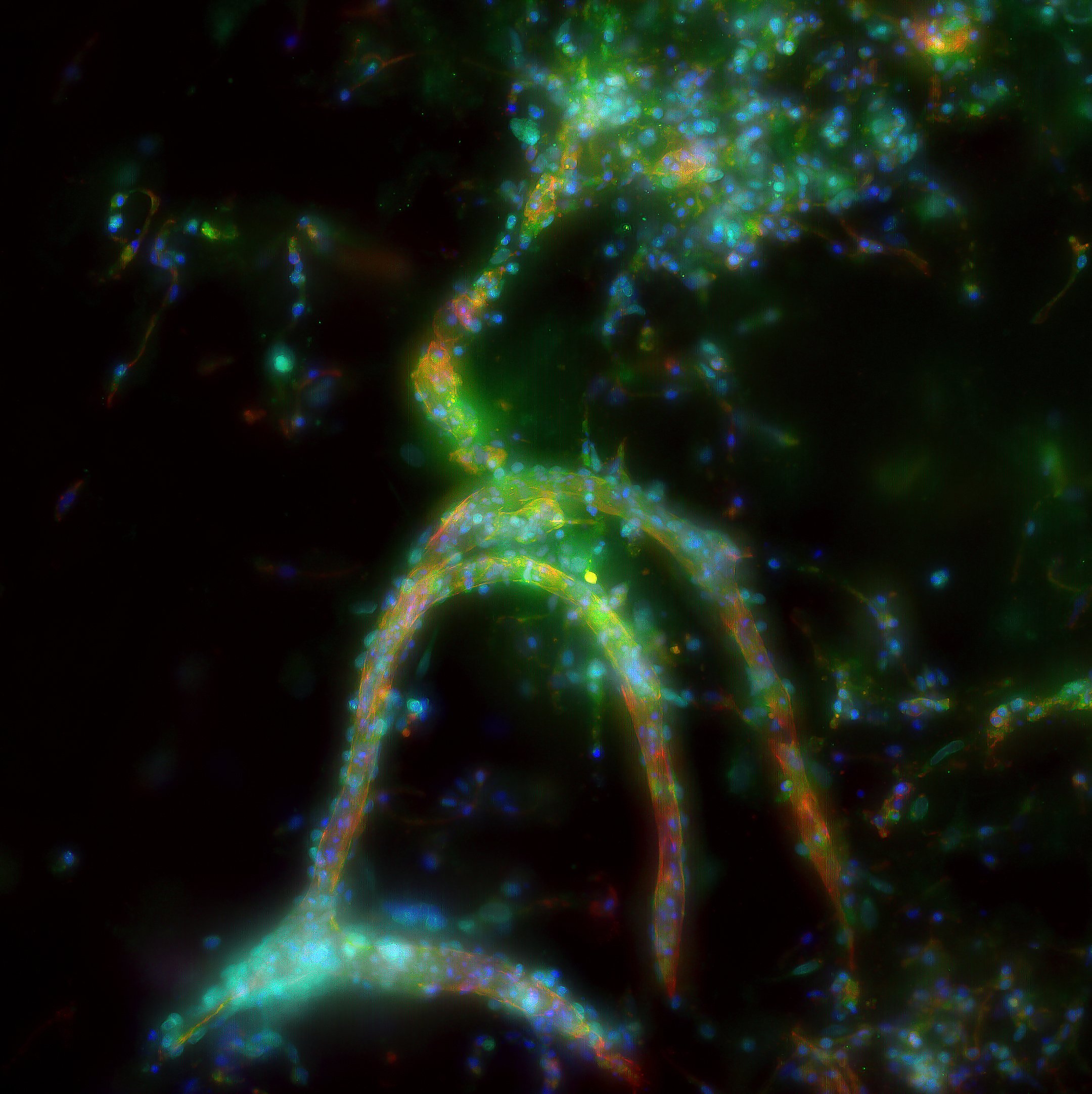
To investigate this, Dr Bosio and her multidisciplinary team of biomedical scientists and engineers are developing a pioneering laboratory model of human microvessels. By growing human microvasculature in the lab, the team can closely observe how sepsis disrupts blood flow and damages vessel function over time.
A key focus of the project is developing advanced microscopic techniques to visualise and record changes in microvessels as they occur. By watching how sepsis alters these vessels in real time, researchers can gain unprecedented insight into microvascular dysfunction, one of the most critical yet poorly understood aspects of the condition.
This approach allows researchers to test potential treatments and interventions in a controlled laboratory environment, providing clinicians with a powerful new tool to evaluate therapies before they reach patients.
By deepening our understanding of how sepsis affects the body at a microvascular level, this research represents an important step toward more targeted, effective treatments. Ultimately, it aims to improve clinical care and reduce the devastating toll sepsis continues to take on patients and families.
This project is made possible through a $20,000 donation given in memory of Margaret Alison Melvin. Philanthropic support like this enables vital research that has the potential to save lives and transform patient outcomes.
Each year, sepsis claims the lives of around 8,700 Australians, more than prostate cancer, breast cancer, or road accidents.
It can strike suddenly, turning what begins as a simple infection into a life-threatening emergency. Survivors are often left with lasting health issues and little understanding of what happened to them.
Sepsis occurs when the body’s immune response to an infection spirals out of control, triggering widespread inflammation, organ failure and, too often, death. Despite its severity, there is still limited evidence to guide the clinical management of sepsis. Current treatments focus largely on managing symptoms through antibiotics, fluids and medications to support blood pressure, rather than addressing the underlying disease processes themselves.
This is where a RPH Research Foundation-funded research project is making a critical contribution.
Led by Dr Erika Bosio, the project focuses on understanding what happens to the body’s microvasculature, the smallest blood vessels in the body, during sepsis. These tiny vessels play a vital role in maintaining circulation and delivering oxygen to organs, yet they are among the first systems to fail when sepsis takes hold.
To investigate this, Dr Bosio and her multidisciplinary team of biomedical scientists and engineers are developing a pioneering laboratory model of human microvessels. By growing human microvasculature in the lab, the team can closely observe how sepsis disrupts blood flow and damages vessel function over time.
A key focus of the project is developing advanced microscopic techniques to visualise and record changes in microvessels as they occur. By watching how sepsis alters these vessels in real time, researchers can gain unprecedented insight into microvascular dysfunction, one of the most critical yet poorly understood aspects of the condition.
This approach allows researchers to test potential treatments and interventions in a controlled laboratory environment, providing clinicians with a powerful new tool to evaluate therapies before they reach patients.
By deepening our understanding of how sepsis affects the body at a microvascular level, this research represents an important step toward more targeted, effective treatments. Ultimately, it aims to improve clinical care and reduce the devastating toll sepsis continues to take on patients and families.
This project is made possible through a $20,000 donation given in memory of Margaret Alison Melvin. Philanthropic support like this enables vital research that has the potential to save lives and transform patient outcomes.